Biology of COVID-19 Disparities
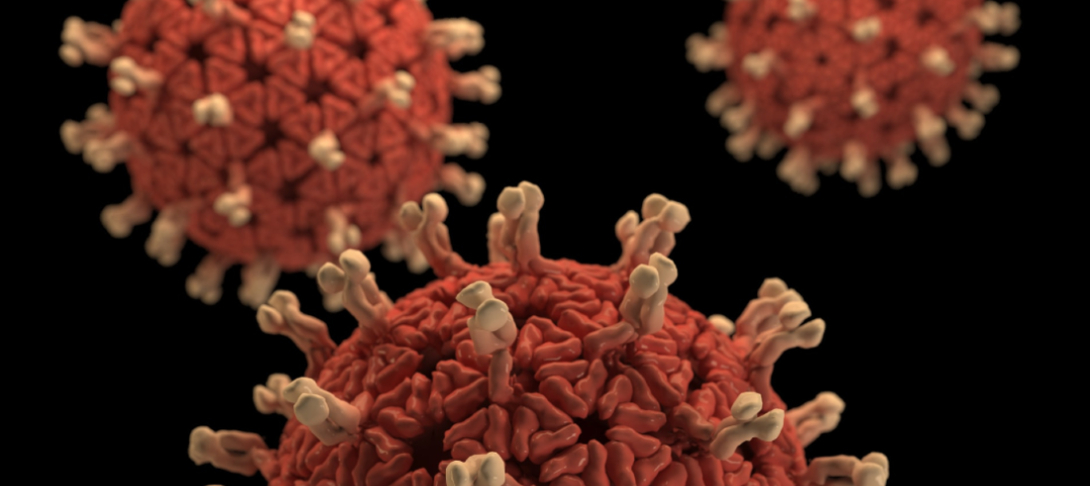
In light of the ethnic disparities seen in disease severity and deaths due to COVID-19, it’s been suggested that perhaps communities of color, or African Americans specifically, have a more pronounced immune response to the SARS-CoV-2 virus, or possess genetic variants that confer greater risk either for individuals to become infected or to become afflicted with more severe disease symptoms.
While many African Americans do show elevations in markers of immune system function, this isn’t the whole story. For example, studies often find that African Americans have greater density of certain receptors on immune cells, elevated antibody production in response to immunization, and higher numbers of Natural Killer cells (responsible for preventing cell to cell spread of virus). However, several studies have also reported diminished immune system function. For instance, studies consistently report that African Americans have lower numbers of circulating monocytes (important for producing and responding to inflammation), as well as lower numbers of circulating neutrophils (important for fighting large pathogens like worms and bacteria.) Currently, the relative importance of these differences, if any, to the disparities seen at the population level with respect to COVID-19 disease is unclear.
With respect to specific genetic variants conferring greater risk of more severe disease once infected, a recent study comparing the protein expression profile of a predominantly Caucasian American subject cohort with a predominantly African American subject cohort found the expression levels of several circulating blood proteins varied with the presence of genomic variants near the coding region for the enzyme determining ABO blood type. For both cohorts, levels for 23 different proteins were significantly associated with genomic variants in this region, but several other associations were significant only for one cohort or the other. Among the proteins upregulated in African Americans according to variants found within the ABO locus was DC-SIGN, a protein used by dendritic immune cells to attach to foreign particles encountered in the body. Using DC-SIGN dendritic cells latch on to bacteria, viruses, and fungi then ingest and digest them into pieces to present to other immune cells responsible for launching an immune response directed toward these fragments. While this pathway is generally protective for an individual, some viruses including HIV and SARS-CoV-1 (better known as SARS) have demonstrated the ability to use this uptake and presentation route as a way to spread infection to cells outside of the lungs. Because the SARS-CoV-1 virus is very similar to the SARS-CoV-2 virus, this could mean that that the DC-SIGN protein functions in context of COVID-19 disease to pass SARS-CoV-2 virus to other cell types. Thus, differential expression of this protein on immune cells between populations could help to account for differences in disease severity across individuals. That said, this mode of intercellular transmission has yet to be demonstrated using SARS-CoV-2 virus in the lab or among patients experiencing COVID-19 disease.
Additionally, because the cohorts compared in this study also differed with respect to prevalence of hypertension, obesity, and diabetes mellitus, the differential expression of proteins such as DC-SIGN could reflect cohort differences in ongoing immune system response to the presence of these chronic conditions rather than implying higher risk to individuals possessing certain genetic variants. It is also important to emphasize that since SARS-CoV-2 virus uses the recently discovered ACE-2 receptor to enter cells, any involvement of the DC-SIGN receptor will likely play a role only after an individual is already infected. Thus any effect differences in DC-SIGN expression has on modifying disease outcomes is only secondary to factors that increase exposure to virus such as crowded living spaces.
In contrast to these race/ethnicity-focused hypotheses, a stress perspective of the disparities witnessed in the current in COVID-19 deaths and disease proposes all individuals with chronically high stress levels (due to discrimination, economic adversity, etc) are at elevated risk of infection and experiencing COVID-19 symptoms as a result of higher circulating cortisol levels. Cortisol, a hormone released into the blood stream during prolonged physical or mental stress, helps to ensure the body can escape or meet the demands of prolonged stressors in part by blunting the release of inflammatory molecules that cause pain, redness, swelling, and immobility. However, in addition to blocking the production and release of these inflammation mediators, it suppresses a number of other immune cell functions including the release of signaling molecules that direct the immune system to begin protecting against viruses specifically. In fact in a landmark study where 389 individuals experiencing ongoing psychological stress were exposed to one of five different respiratory viruses, susceptibility to viral infection was found to vary according to the level of psychological stress experienced by study subjects, with higher levels of stress placing individuals at greater risk of infection by any of the viruses tested.
Currently, there is not enough information to determine if any of these effects significantly influence COVID-19 disease progression or outcomes in real patients. As more information regarding SARS-CoV-2 and COVID-19 disease becomes available please check back with us to learn more.
Related Links
- Christy, C., Pichichero, M. E., Reed, G. F., Decker, M. D., Anderson, E. L., Rennels, M. B., Englund, J. A., Edwards, K. M., & Steinhoff, M. C. (1995). Effect of gender, race, and parental education on immunogenicity and reported reactogenicity of acellular and whole-cell pertussis vaccines. Pediatrics, 96(3 Pt 2), 584–587.
- Cohen, S., Tyrrell, D. A., & Smith, A. P. (1991). Psychological stress and susceptibility to the common cold. The New England Journal of Medicine, 325(9), 606–612.
- Elenkov, I. J. (2004). Glucocorticoids and the Th1/Th2 Balance. Annals of the New York Academy of Sciences, 1024(1), 138–146.
- Hoffmann, M., Kleine-Weber, H., Schroeder, S., Krüger, N., Herrler, T., Erichsen, S., Schiergens, T. S., Herrler, G., Wu, N.-H., Nitsche, A., Müller, M. A., Drosten, C., & Pöhlmann, S. (2020). SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell, 181(2), 271-280.e8.
- Katz, D. H., Tahir, U. A., Ngo, D., Benson, M. D., Bick, A. G., Pampana, A., Gao, Y., Keyes, M. J., Correa, A., Sinha, S., Shen, D., Yang, Q., Robbins, J. M., Chen, Z.-Z., Cruz, D. E., Peterson, B., Natarajan, P., Vasan, R. S., Smith, G., … Gerszten, R. E. (2020). Proteomic Profiling in Biracial Cohorts Implicates DC-SIGN as a Mediator of Genetic Risk in COVID-19. MedRxiv: The Preprint Server for Health Sciences.
- Malat, G. E., Culkin, C., Palya, A., Ranganna, K., & Kumar, M. S. A. (2009). African American kidney transplantation survival: The ability of immunosuppression to balance the inherent pre- and post-transplant risk factors. Drugs, 69(15), 2045–2062.
- Yang, Z.-Y., Huang, Y., Ganesh, L., Leung, K., Kong, W.-P., Schwartz, O., Subbarao, K., & Nabel, G. J. (2004). pH-Dependent Entry of Severe Acute Respiratory Syndrome Coronavirus Is Mediated by the Spike Glycoprotein and Enhanced by Dendritic Cell Transfer through DC-SIGN. Journal of Virology, 78(11), 5642–5650.
- Yi, J. S., Rosa-Bray, M., Staats, J., Zakroysky, P., Chan, C., Russo, M. A., Dumbauld, C., White, S., Gierman, T., Weinhold, K. J., & Guptill, J. T. (2019). Establishment of normative ranges of the healthy human immune system with comprehensive polychromatic flow cytometry profiling. PLoS One, 14(12), e0225512.